
Cancer Vaccines are Extending the Lives of Cancer Patients
Excellent data across multiple types of cancer.
Bone trauma increases risk of metastasis, including osteoporosis and micro-fractures
-

18% increased risk of bone metastasis
Cancer growth and recurrence can be triggered by bone fractures. Although this may seem like a recent discovery, the medical community has recognized this connection for over 100 years. A 2022 observational study of 84,300 breast cancer patients in Germany revealed a significant link between bone fractures and an increased risk of metastasis—showing a 12% rise in recurrence risk (RoR). The risk was highest in patients with bone metastases (18% RoR), followed by those with metastases in other distant organs (16% RoR). While this study focused on breast cancer, similar patterns have been observed in other research studies with several different cancer types, reinforcing the critical role of bone trauma in cancer progression.
-

Bigger trauma has higher risks
Severe bone fractures or trauma increase risks of recurrence. According to Dr. Xiang Zhang and current research, larger bone trauma, like a significant fracture or surgery involving bones, is associated with an increased risk of cancer recurrence, particularly for cancers prone to bone metastasis, such as breast and prostate cancers. Trauma can create a microenvironment that promotes cancer cell migration and establishment in the bone, leading to a higher likelihood of the cancer returning to that site. However, don’t let fear of bone breaks slow you down because exercise provides a significant 30-50% risk reduction in recurrence of cancer. Bubble-wrapping yourself isn’t a solution; I’m still skiing but now I take a little more care on the black diamonds.
-

Recurrence usually occurs within 3 years
Cancer recurrence resulting from bone trauma can occur very quickly. Dr. Xiang Zhang explains that if there will be a recurrence due to bone trauma, it usually occurs within the first three years and often is seen as early as the first year after the event. Patients can use this information to request follow-up screening to identify any recurrence quickly and receive prompt treatment. Lower tumor burden is usually associated with better prognosis, so addressing an issue right away is important. Don’t let scanxiety keep you from critical information that could help your outcome. Talk to your doctor about enhanced screening and the use of drugs to reduce the bone-turnover rate which could minimize risk of recurrence and improve outcomes.
Latent cancer cells are cancer cells that are present in the body but are not yet causing symptoms or growing into a tumor. These cells can remain dormant or “asleep” for months or even decades. They are sometimes referred to as Cancer Stem Cells because they have stem cell-like properties and they often survive traditional chemotherapies, hiding in microvasculature or bone marrow.
Research indicates that bone fractures can "wake up" latent cancer cells by releasing growth factors and inflammatory signals that promote cancer cell growth. This phenomenon is primarily due to increased bone turnover rates associated with the healing process.
Bone fracture can “wake up” latent cancer cells
Bisphosphonates,
an Anti-Cancer Strategy
Bisphosphonates are a class of drugs that can be used to slow down the bone turnover rate which reduces the risk of cancer recurrence, metastasis, and skeletal-related complications of cancer for postmenopausal breast cancer and perhaps other cancers as well including lung.
A meta-analysis of randomized breast cancer trials found that bisphosphonates not only reduce the risk of breast cancer recurrence in bone for early stage disease but also improves survival in postmenopausal women when used as adjuvant therapy. Specifically, the use of bisphosphonates was associated with a 25% reduction in the risk of breast cancer recurrence in bone and an 18.3% reduction in breast cancer mortality over the first decade after diagnosis in postmenopausal women (study link).
Dr. Xiang Zhang, PhD
Baylor College of Medicine
Director, Lester and Sue Smith Breast Center and William T. Butler, M.D., Endowed Chair for Distinguished Faculty
Prior to his appointment at Baylor, Dr. Zhang completed a post-doctoral fellowship at Memorial Sloan-Kettering Cancer Center and received his Phd from Columbia University. He is widely-published in top-tier medical journals and has received numerous honors and awards.
Era of Hope Scholar (Dept. of Defense, 2010-2014)
NIH Pathway to Independence Award (National Cancer Institute, 09/2010 - 09/2014)
Excellence in Research (Department of Molecular and Cellular Biology, BCM, 08/2016).
Bisphosphonate
Details
-
Research indicates that nitrogen-containing bisphosphonates (N-BPs) may be beneficial in a cancer setting. Popular N-BPs include…
Alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), pamidronate (Aredia), and zoledronic acid (Zometa).
-
Bisphosphonates are a prescription from your doctor. Ask them if it might be right for you.
It is usually covered by insurance for cancer patients.
-
The dosing frequency varies by drug and by individual case.
When I first started using a bisphosphonate, I was in chemotherapy and I received it every 6 weeks. After chemotherapy was over, I transitioned to 4x a year. After two years, I began receiving it 2x per year.
Talk to your doctor to find a frequency that is right for you.
Denosumab doesn’t provide the same anti-cancer benefits
Denosumab (Xgeva) doesn’t provide the same anti-cancer benefit as bisphosphonates (e.g. Zometa) even though it may have superior abilities to build bone.
“Denosumab, which has similar effects on bone cell physiology, appears not to consistently influence disease outcomes, perhaps suggesting that it is the “off target” effects of bisphosphonates on immune function and the biological processes involved in metastasis that are important.”
Xiang Zhang Lab
The laboratory of tumor ecosystems and metastasis, Dr. Zhang’s lab focuses on breast cancer bone metastasis and tumor immunology. It is currently developing a new targeted drug that utilizes bisphosphonates to fight bone metastasis.
Xiang Zhang Lab Recent Discoveries
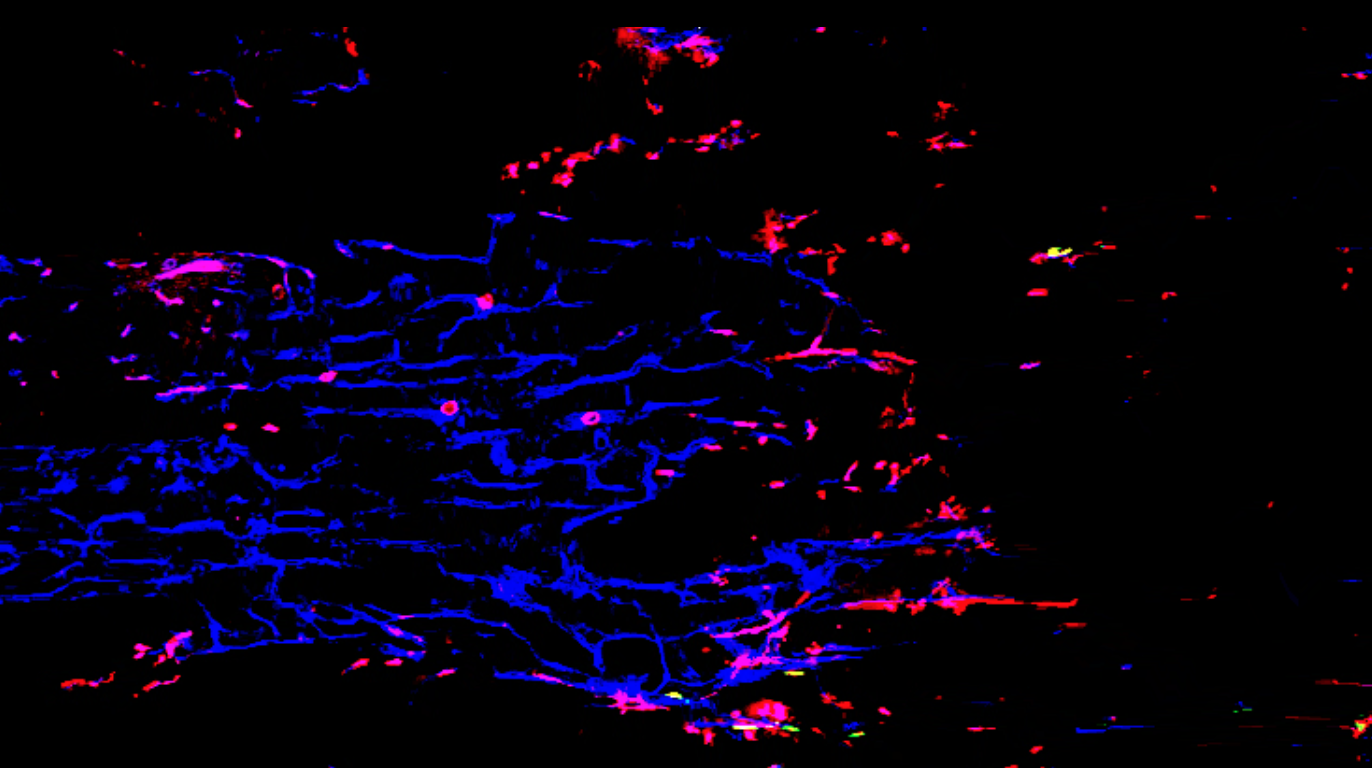
Even before tumor metastasis, breast cancer remotely induces changes to immune cell development in the bone marrow; new findings show three discrete subgroups of B cells that influence the changes.
To create medical breakthroughs, Zhang’s lab first needed to invent a way to watch healthy cells interact with cancer cells during metastasis. They developed a process called Sortase A-Based Microenvironment Niche Tagging (SAMENT). SAMENT allowed them to see compromises in the immune cells that occur before metastasis. LINK TO STUDY
Only 15 to 20% of triple negative breast cancer patients will benefit from immunotherapy treatment; new research helps identify who will benefit.
Two newly discovered, distinct patterns of B cell abnormalities could serve as blood biomarkers for determining likelihood of response to standard-of-care chemotherapy and immunotherapy. LINK TO STUDY
Zhang Lab identified three unique mechanisms used by different cancer types (breast, lung, kidney) to metastasize to the bone; this discovery is leading to new interventions for prevention of spread and recurrence in bone
Bisphosphonates and denosumab (anti-RANKL) have been widely used to treat bone metastases of various cancer types, including osteosclerotic prostate cancers. However, some cancers do not respond to these agents. Renal cancers, for instance, are notoriously resistant to bisphosphonates despite the similar osteolytic appearance, suggesting potentially osteoclast-independent mechanisms.
This pivotal research elucidates the immunosuppressive mechanisms in bone metastases. The Zhang Lab demonstrates how different cancer types may colonize the same organ via a finite number of distinct mechanisms, and provides rationale to investigate completely different treatment strategy for certain bone metastases. LINK TO STUDY







